STOCKHOLM, Sweden — Whether continuous glucose monitoring (CGM) is for “everyone” — and if not, for whom — was the subject of heated debate at the recent 2022 annual meeting of the European Association for the Study of Diabetes (EASD).
During the discussion, both participants generally agreed that CGM is appropriate for all people with type 1 diabetes and those with type 2 diabetes on intensive insulin regimens.
Most of the discussion has focused on people with type 2 diabetes on less intensive treatments and other subgroups.
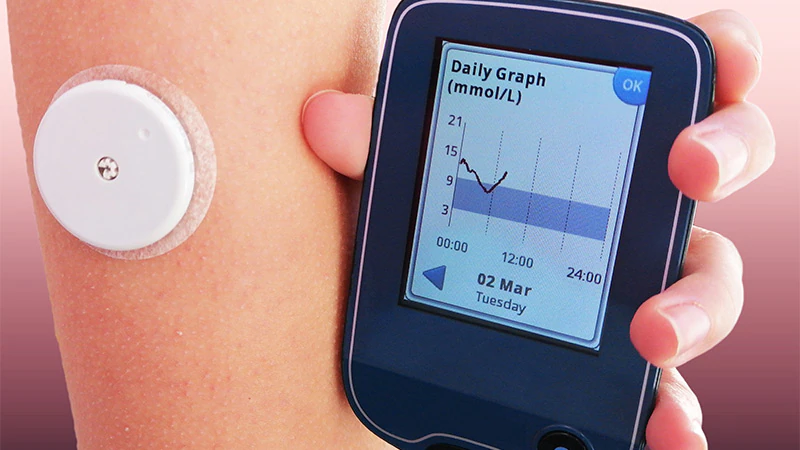
The use of CGM is growing
Maciej T. Malecki, MD, PhD, of the Department of Metabolic Diseases, Jagiellonian University Medical College, Krakow, Poland, supported the “yes” side. He observed, “CGM is not a tool for all patients with diabetes. However, large groups of patients with diabetes benefit from its use. The use of CGM will increase rapidly as new technologies develop and prices fall.
He began by listing the benefits of CGM, including improved glycemic control, safety in the form of alarms for low glucose levels, avoiding the drawbacks of fingertip glucose monitoring, and the ability of CGM to enable closed-loop insulin delivery, also known as artificial pancreas systems.
There is a lot of literature at this point on the benefits of CGM in type 1 diabetes. Just today a new study was just published in the New England Journal of Medicine detailing the results of the FLASH UK study. In the trial, among 156 participants with type 1 diabetes and an average baseline A1c of approximately 8.6%, those randomized to FreeStyle Libre 2 (Abbott Diabetes Care) intermittent scanning experienced lower 0.5 percentage point higher A1c at 24 weeks compared to usual finger blood. blood sugar test (P < 0.001), and they spent 43 minutes less time in hypoglycemia per day.
In Stockholm, Malecki described a 7-year follow-up study published in January showing that starting CGM within a year of being diagnosed with type 1 diabetes leads to long-term improvement in A1c compared to starting later or not at all. And another trial reported in 2019 found that it is real-time (i.e. not intermittently scanned) CGM, regardless of insulin delivery method (pumps or injections), that makes a therapeutic difference in people with type 1 diabetes.
And earlier this year, a systematic review and meta-analysis of randomized controlled trials confirmed the superiority of CGM for monitoring the fingertip in people with type 1 diabetes, particularly those with baseline levels of A1c are greater than 8% (64 mmol/mol).
In pregnant women with type 1 diabetes, the CONCEPTT randomized controlled trial showed better outcomes in terms of neonatal birth weight and length of infant hospitalization with the use of CGM compared to monitoring by finger picking.
For people with type 2 diabetes, in the DIAMOND trial, adults aged 60 years and older with type 1 (n=34) or type 2 (n=82) diabetes receiving multiple injections both saw reductions in A1c with CGM.
Meanwhile, in a single-arm study of adults with type 2 diabetes treated with only basal insulin or non-insulin therapy, using CGM for 6 months significantly improved time in range and A1c, regardless of how many medications patients were taking. . The authors of this study write that their data and others suggest that “insurance eligibility criteria should be changed to expand the use of real-time CGM by type 2 diabetic patients treated with therapies less intensive.
And in data from the German real-world registry, which included 1440 adults with type 2 diabetes, in patients not on intensive insulin therapy (78%), initiation of CGM resulted in significant reductions in A1c, body mass index and severe hypoglycemia. These authors concluded that CGM use “may be associated with improved treatment adherence, dietary changes, and increased physical activity with CGM readings.”
Evidence also supports the use of CGM in hospitals, including a recent randomized trial of general practice and surgical inpatients with type 1 or type 2 diabetes on insulin, which showed significant reductions in hypoglycemia using CGM to guide insulin adjustments compared to those on the verge of care resulting in significantly fewer episodes of hypoglycemia.
Malecki also reviewed data showing benefits of CGM on maternal and neonatal outcomes in gestational diabetes, older adults with memory problems, transient neonatal diabetes, and diabetes secondary to radical pancreatectomy.
He concluded: “There is a growing body of evidence that CGM also improves glycemic control in type 2 diabetes with less intensive hypoglycemic treatment. Further data, including cost-effectiveness and quality of life, are needed. However, it can be expected that the use of CGM in this patient group will increase.”
How compelling is the data for those who do not take insulin?
Taking the opposite position, J. Hans DeVries, MD, PhD, Professor of Diabetes Medicine, Stockholm University, Sweden, began by citing a real-world retrospective, data analysis, of which Malecki was lead author, which found patients in Poland generally scan intermittently scanned CGMs more often and achieve lower A1c levels and longer journey times than people with diabetes in other parts of the world.
“It’s the Polish doctors. They’re just better than us,” he joked.
He agreed with Malecki that all patients with type 1 diabetes should be offered CGM, citing the American Diabetes Association/EASD Consensus Report on the Management of Type 1 Diabetes in Adults, which states that this is the standard of care.
However, he pointed out that while most patients with type 1 diabetes can benefit from CGM, some will choose not to use it. “It’s not suitable for everyone. Some might not find it helpful. They might find it stressful because they don’t like being strapped to a device or being constantly reminded of their diabetes or feeling feel exhausted from the alarms.”
He also agreed that CGM is “a closed case” for people with type 2 diabetes who are on basal-bolus insulin therapy, noting that these people “are not fundamentally different from type 1 patients, it is therefore logical that for these patients, CGM is very useful.”
But for people with type 2 diabetes who only take basal insulin, DeVries said the data is less compelling. For example, in a randomized trial of 175 such patients, there was a significant difference of 0.4 percentage points in A1c attainment between those randomized to CGM versus fingertip glucose monitoring. However, in the supplement, 24-hour data showed no difference in fasting glucose levels or total daily insulin dose, suggesting that “these patients did not use more insulin due at CGM…it’s a behavioral intervention.”
And now, DeVries pointed out, a study in which tirzepatide, a new once-weekly injectable agent for type 2 diabetes, was added to insulin glargine in patients with type 2 diabetes suggests an alternative to CGM, as this diet produced a greater drop in A1c (–1.47 versus –0.4 percentage points) as well as significant weight loss (–10.5 kg versus no change) and no alarm. “It’s not a hard choice,” he commented.
Regarding people with type 2 diabetes who are not on insulin, DeVries pointed to a study from Japan that showed a significant drop in A1c in those using flash glucose monitoring compared to monitoring at your fingertips. However, a third of those who were assessed for eligibility declined to participate, and of the remaining 100 patients who were randomized, the difference between the groups in A1c was only 0.29 percentage points.
“We have to ask ourselves how significant is this difference? I don’t think the data is very compelling for patients who are not on insulin. And that is, of course, the most important group,” said he noted.
As for people without diabetes or with prediabetes, he pointed out that the market is potentially huge, as long as the device is non-invasive.
Smartwatches are being developed for all sorts of medical assessments, including heart rate, blood pressure, temperature, sleep patterns, gait, and mobility, in addition to glucose and insulin resistance. ‘insulin. About 50 million Americans currently use a smartwatch, he noted.
For people without diabetes, using CGM can reveal how foods affect their blood sugar levels, which could translate to earlier detection of diabetes or prediabetes and possibly healthier behavior. And in fact, DeVries said some key opinion leaders in the field argue that every healthy person should use CGM occasionally. “There is of course a huge problem. It is that we have no data on this.
Malecki said he received fees for his services as a consultant or speaker from Abbott, Ascentia, Dexcom and Medtronic. Her institution is supported by an unrestricted grant from Medtronic. DeVries had no relevant financial relationship to disclose as of September 2021, as he is seconded 4 days a week to the European Medicines Agency. None of the statements he made reflect the views of the agency in any way. In the past it has had disclosures with Abbott, Afon Technology, Dexcom, Lilly, Medtronic and Metronom Health.
Miriam E. Tucker is a freelance journalist based in the Washington, DC area. She is a regular contributor to Medscape, with other work published in The Washington Post, NPR’s Shots blog, and Diabetes Forecast magazine. She’s on Twitter: @MiriamETucker.
For more diabetes and endocrinology news, follow us on Twitter and Facebook.
#continuous #glucose #monitoring #diabetes